
Not long ago, the idea of checking a patient’s vitals from miles away seemed futuristic. But as healthcare faced the dual pressures of rising chronic disease and aging populations, Remote Patient Monitoring (RPM) emerged as a powerful solution—turning home devices into daily health checkpoints and transforming how we think about outpatient care.
Today, RPM is no longer just a pilot project or a nice-to-have. It’s a Medicare-reimbursed, evidence-backed method of improving patient outcomes, reducing avoidable hospitalizations, and helping providers keep pace in the shift to value-based care.
With the entry, and reimbursement of RPM, and years of data underneath us, it’s time to take a look at the data. Has remote patient monitoring proven to be effective?
The Road to Medicare Approval
The formal entry of RPM into mainstream care began in 2018 when the Centers for Medicare & Medicaid Services (CMS) approved CPT code 99091, reimbursing time spent reviewing physiologic data collected remotely.
Since then, CMS expanded coverage with codes 99453, 99454, 99457, and 99458, building a pathway for providers to bill for:
• Device setup and education – 99453
• Data transmission and analysis – 99454
• Monthly patient interaction and intervention – 99457 Initial 20 minutes, 99458 subsequent 20 minutes
CMS was saying, in effect: “RPM works—and we’ll pay for it.”
Why RPM? The Promise That Sparked the Movement
RPM solves some of healthcare’s biggest challenges:
• Managing chronic conditions like hypertension and diabetes
• Helping rural or mobility-limited patients
• Reducing post-discharge complications and readmissions
• Controlling rising healthcare costs
By bringing real-time data into the clinical workflow, RPM makes care continuous and proactive—not reactive.
The Evidence: What the Data Shows
1. Improved Clinical Outcomes
| Condition | Clinical Benefit | Source |
| Hypertension | Avg. 8 mmHg systolic BP drop | The Lancet, 2021 |
| Heart Failure | Up to 50% fewer hospital days | The Lancet, 2018 |
| Diabetes | Avg. 0.5% A1c reduction | JAMA, 2022 |
| COPD/Asthma | Fewer exacerbations and ED visits | Chest, 2021 |
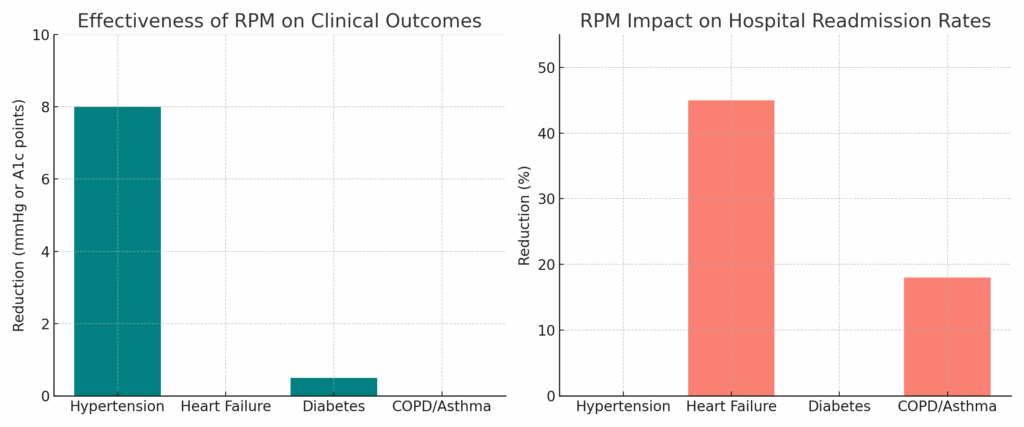
2. Fewer Hospital Visits, More Savings
• 32% reduction in admissions — Health Affairs, 2022
• $312 quarterly savings per Medicare beneficiary — CMS Data
• 18% fewer ED visits — VA Remote Monitoring Program
• 25–50% drop in readmissions for heart failure — TIM-HF2 Trial
3. Patients Actually Like It
• 70–90% compliance with device use
• Greater sense of connection and confidence in care
• Improved engagement and health literacy
“Remote monitoring makes me feel like my doctor is with me every day, not just once a year.” — RPM Patient, Cleveland Clinic
For Providers: A New Model of Care
RPM is especially powerful in a value-based care environment. It helps providers:
• Meet MIPS, HEDIS, and ACO benchmarks
• Prevent avoidable hospital penalties
• Improve patient satisfaction and Star Ratings
• Scale care delivery without sacrificing quality
The Verdict: RPM is Proven. Now It’s Time to Scale.
RPM has moved from emerging tech to essential infrastructure. Medicare backs it. Studies validate it. Patients appreciate it.
RPM was the tip of the spear in providing closer monitoring and additional data that assists in managing high, and higher risk patients on a short term and longer term basis. Remote technology since RPM’s initial usage has grown significantly. It will be exciting to see how much further this will improve not only chronic management but the diagnostic and management capability remotely for patients.
If you’re a healthcare organization looking to improve outcomes while managing risk, the question isn’t whether RPM works—it’s whether you’re ready to make it work for you.
CONTACT US to learn more about how to start or bill for RPM in your healthcare organization.
References
- Omboni, S., et al. (2021). Telemonitoring for Hypertension Management. The Lancet.
- Koehler, F., et al. (2018). TIM-HF2 Trial. The Lancet.
- Green, B. B., et al. (2022). Effect of Home Monitoring in Diabetes. JAMA.
- VA Telehealth Services. (2021). Remote Monitoring Outcomes. VA.gov.
- CMS Innovation Center. Chronic Care Remote Monitoring Demonstration.
